Thursday April 30, 2020 ~ VICTORIA, BC
by Mary Brooke, B.Sc. ~ West Shore Voice News
BC is now 100 days into the COVID-19 pandemic, with 25 new cases today (bringing the total of test-positive cases to 2,112) and 111 deaths to date. Without a vaccine or even a proven treatment, the fight is not over against COVID-19, not by a long shot.
There’s at least one more full respiratory illness season ahead of us (Fall 2020 through Winter 2021 into spring of next year), during which physical distancing and periods of self-isolation will be the required norm. That will come as a mix of more social and economic activity than we’re seeing now, as sector-by-sector the Provincial Health Officer will open up our freedoms to move about again. That will open up the risk to infection. It’s a planned gamble, but it’s a gamble nonetheless.
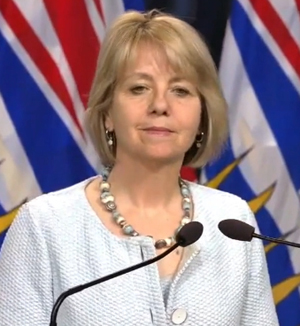
The process of getting started with the ‘new normal’ — as announced earlier this week by Premier John Horgan — will begin next week. One by one, or in small clusters, Provincial Health Officer Dr Bonnie Henry will identify sectors that can go first or be next. She says she will welcome input from various sectors on how her broad guidelines might be implemented.
BC is still in a State of Emergency for two more weeks, as announced yesterday by Premier Horgan.
First steps toward the new normal:
Likely among the first sectors to see some fluidity will be schools, child care, some level of community activity such as summer camps and sports, probably a few more sectors of retail than are presently open. After that, possibly some components of the personal service sector.
Pretty much last on her list will be casinos, Dr Henry said today, even though casinos generate a lot of income for municipalities and community initiatives. She outlined a number of the risk factors that apply across the board for all sectors — starting with how essential something is to the economy and society, and then mostly to do with proximity of people (i.e. can physical distancing be achieved) and age factors (with older persons still considered most susceptible to acquiring or suffering the worst from the COVID-19 viral infection).
That sort of phased process not only takes advantage of the intel of the many economic sectors but somewhat assures buy-in, as the ideas will not be imposed by Dr Henry but will have been generated from within each sector of community, business or industry as the big freeze of social-isolation begins to be thawed.
The process is ideally slow and carefully done. But life is life… with a mind of its own… and it will take — as Health Minister Adrian Dix repeats often — for “everyone to be 100 percent all in” to maintaining that flattened curve (slow rate of COVID-19 infection that does not overwhelm the health care system) in BC.
The new normal is something that will evolve. The pandemic is still active and could get worse if people let up their resolve to physically distance and self-isolate. People still get sick from COVID-19 every day, impacts on the economy have been massive, and the aftermath of mental health responses (due to emotional, social and financial loss and crises) over months and years to come will have indelible impacts.
BC-style pandemic response:
Provincial Health Officer Dr Bonnie Henry refers to the province-wide experience of dealing with the novel coronavirus called COVID-19 as “our pandemic” — the way she and the government want to deal with the situation in this province.
BC has clearly come out ahead of most other jurisdictions in Canada if not the world in terms of containing the spread of COVID-19 infection. That’s if you look at the overall total numbers compared to other provinces and countries.
It does mean that British Columbians have — for the most part – been “all in” to the commitment to self-isolate and practice physical distancing, in addition to the other standard good hygiene measures of washing one’s hands and sneezing away from others or into a tissue or sleeve. The new mantra for all of us is “to stay home if you’re ill”.
Today Minister Dix and British Columbians by default enjoyed some national accolades on national TV, in the hour ahead of his joint near-daily COVID-19 media session with Dr Bonnie Henry. On the CTV political news show Power Play, host Evan Solomon asked Dix how it is that BC has done so well in containing the spread of COVID-19.
Dix said BC has seen a flattening of the curve “because from January we’ve taken a systematic approach and because the people of BC have just been extraordinary in putting in place physical distancing measures”. With a systems perspective, Dix highlighted that BC reached a one-day high of 149 people in hospital with COVID-19, compared to 87 yesterday (and a high of 72 in critical care at one point, compared to 35 on April 29).

“The new normal is not like the old normal,” said Dix. “We’re still going to require rules, industry by industry.” He pointed out how the construction industry was not shut down in BC, but worked within rules so they could continue to function in a protected way.
Reviewing the workplace/illness relationship:
On that point of staying home when ill, it has been clear that going to work when sick — out of necessity to make ends meet — indicates a cost of living challenge to many and underscores the need for an improved social safety net (such as a guaranteed living allowance, similar to the Canada Emergency Response Benefit which offers one flat amount).

This month that shortfall in the economy (i.e. people doing whatever it takes to make money, because they have to for survival) was highlighted by where a large number of test-positive cases of COVID-19 have shown up.
Two poultry processing plants (one in Vancouver, and the other in Coquitlam) together as of today have 92 test-positive cases. Some people had gone to work even when ill, and their infection of COVID-19 had spread. As well, Dr Henry today said that food safety inspectors had not also checked for work-safe conditions.
Close-quarters allows more opportunity for infection:
As was seen first with the cruise ships where hundreds of people acquired COVID-19, contained living spaces are ideal for incubation of the virus.

There has also been a virulent outbreak in the close-quarters of the federal medium security Mission Institution in the BC interior, where 120 people (both inmates and staff) have tested positive, and one inmate died on April 15. This is evidence of a direct correlation of communal living with the spread of this disease.
Which highlights the darkest shadow of BC’s COVID-19 experience: the primary location of infectious outbreaks has been in long-term care homes where communal living is the current setup. Residents in great number (as well as staff) have become ill with the virus: so far that’s 256 residents and 153 staff, said Dr Henry today. At least 24 long-term care homes have been impacted during the pandemic so far.
A focus on long-term care homes:
Most of the 111 deaths in BC from COVID-19 have been in the long-term care homes and assisted living facilities. This has cast a harsh light on problems with social care attitudes toward seniors, as reflected in the low wages in that sector and that care homes have long been able to get away with part-time contract scenarios without benefits.
Setups of communal living may not be ideal, yet housing accommodation is costly. If long-term care homes are to be more spacious, that will take a lot more government funding, as not the majority of seniors or their families will have enough resource to pay for long-term care themselves.
Dr Henry has said that much of the ‘fix’ for the issue of cross-contamination that has resulted from workers taking work in more than one long-term care facility is to pay the workers more.
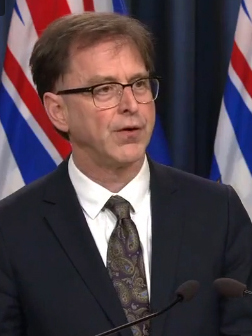
In the meantime, a few weeks ago BC Health Minister Dix brought forward instructions and $10 million to facilitate the process of long-term care workers arranging employment at just one location now and going forward.
Dix said today that 276 facilities out of 545 in BC that hosted multiple-facility employees had completed their transition (a single-site plan) in that regard. He said that 7,350 workers have been working at jobs in multiple facilities (103 in the Vancouver Coastal Health Authority, 64 in Island Health, 43 in Interior Health, 40 in Fraser Health, and 26 in Northern Health). “More completions expected next week,” he said.
Hospital readiness and non-COVID care:
There are 82 people are in hospital today with COVID-19 in BC, down from a high of 149 (on April 6). There are still 4,100 available hospital beds to accommodate an influx of COVID-19 patients, which shows 63.2% current utilization; current occupancy of critical care units is 44.6%.
As a slow way of inching toward the new normal in the health care system, Dix is starting to encourage people to use the health care system for health needs that are not related to COVID-19. His indicator for public confidence in using the health care system is the number of visits to emergency rooms in BC. Yesterday that number was 4,481 visits, which continues to be higher than it was at the low of 2,995 a few weeks ago. The largest volume was seen as 6,559 cases on March 9 which was still pre-pandemic. Numbers of visits to the ER are “still below that, but people are returning and we appreciate that”, said Dix.
Although there has been no known discussion of whether some people realize they can manage without a visit to the ER, while they’ve been taking care of things in self-isolation or with other sorts of care or remedy. If for anyone there has been a knee-jerk reaction to dash off to ER as the first point of entry to the health care system, perhaps COVID-19 has made people pause to think about that approach or about other forms of care and treatment.