Monday July 6, 2020 ~ VICTORIA, BC
by Mary Brooke, B.Sc., editor ~ West Shore Voice News
BC’s public health star Dr Bonnie Henry is herself a big fan of the World Health Organization (WHO). And she certainly stuck up for the organization that she participates in directly, in response to a query about a recent report that suggests the COVID-19 virus is spread more easily through the air than has been thought to be the case so far.
This could have implications for how long people remain in a room, or in confined scenarios like long flights on airplanes.
If that’s the case, it challenges the entire premise that physically distancing by two metres (six feet) is enough to achieve being out of the line of direct transmission of the ‘large moist droplets’ from coughing, sneezing and speaking or singing that have been shown to project the virus through the air.
WHO says 1 metre is enough:
In fact the WHO states to only “maintain at least 1 metre (3 feet) distance between yourself and others” (which is half of what public health is telling people in Canada and most western countries).
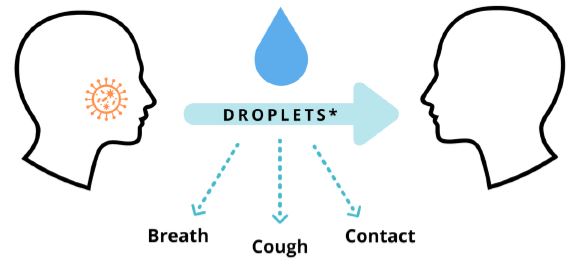
WHO states: “When someone coughs, sneezes, or speaks they spray small liquid droplets from their nose or mouth which may contain virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person has the disease.” | Advice for individuals to prevent COVID-19 spread (WHO)
As much as a cheerleader as a medical professional, BC Provincial Health Officer Dr Henry said defensively that the World Health Organization “has been doing an amazing job at trying to keep up with what is going on. The report that I saw… I don’t think they presented the WHO perspective … (they were) trying to foment a bit of controversy.”
That’s as if to say that WHO is the ultimate authority on all things COVID-19, even though over the course of this year they have even admitted to being slow on recommending the use of non-medical masks, let alone their tardiness in declaring COVID-19 as a pandemic (though there were arguably political reasons for that at the time).
Respiratory viruses are carried in droplets:
If there is some validity to the idea that smaller droplets containing the COVID-19 virus can be spread through the air over a longer period of time compared to the heavier droplets spread more directly when in the immediate proximity of infected persons (asymptomatic or otherwise), that sets public health in BC once again to consider revising its recommendations to individuals, families, businesses and organizations.
Dr Henry continued, saying that the discussion of how respiratory illness is spread “has been an ongoing discussion for many many years”

“COVID is only one,” she said, adding that “many of these discussions have been around influenza in particular”, about the “gradation of how droplets come out” when people cough, sneeze or talk.
Referring to the size of moist droplets: “Small ones get into the lung, large ones into the back of throat or upper part of lungs,” said Dr Henry. “They are airborne transmitted…. very small particles that can last in the air for many hours,” she said.
“They float in an air column, such as down the hallway or through the ventilation system,” she explained, noting that viruses like measles can travel that way and also the bacteria that causes tuberculosis.
“Viruses like COVID-19 and influenza transmit in larger droplets when you’re close to somebody,” said Dr Henry. She continued by explaining that “we find some smaller droplets” and that there is a range of sizes of droplets when somebody’s talking.
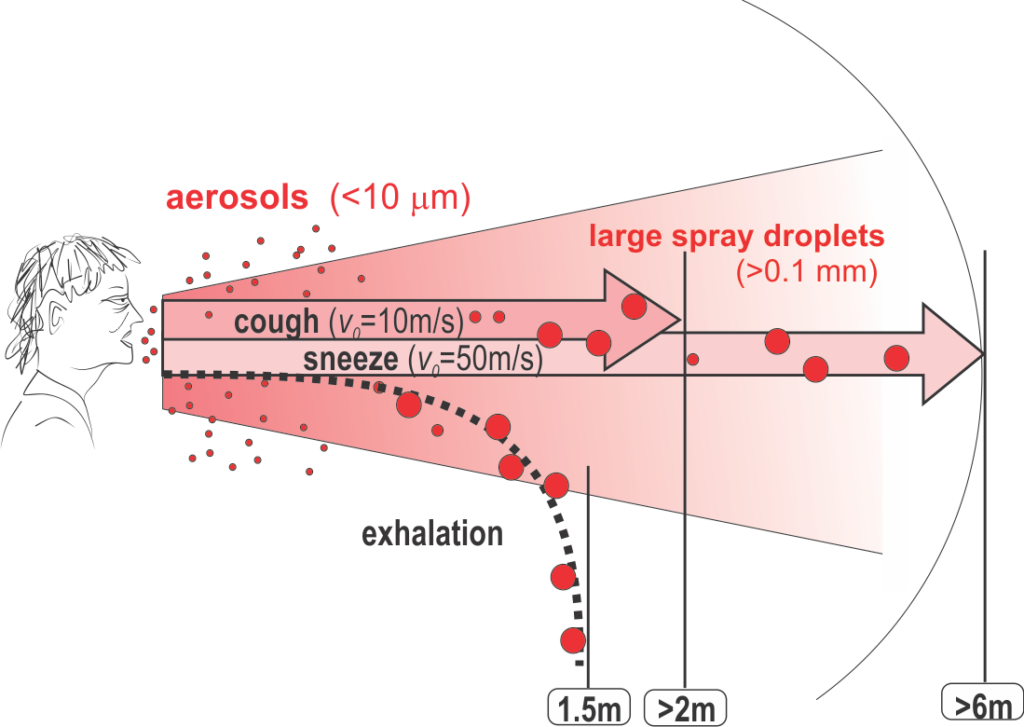
The COVID-19 and influenza viruses need moisture “a bit more” to stay alive compared to other airborne disease-causing microbes. She said that everyone in public health is “on the same page” as to the virus being transmitted through air and that they can’t survive “for long distances in an air column”.
Getting a handle on spread:
The challenge is to understand how much spread is due to the small aerosols compared to the large droplets that tend to fall out more readily. “How much goes deep into my lungs and how much is deposited in the upper airway” is the question, said Dr Henry.
In a health care setting with COVID or influence “it is incredibly important to do a hierarchy of controls”, she explained, including use of masks, minimizing time in the room, doing impeccable hand hygiene, and using eye protection… “all of those things that we have in place that protect people”.
Close contact is a key part of the equation:

“When you’re in close contact within two metres or one metre, if you’re indoors with poor ventilation, when there is coughing, sneezing,
singing (see University of Alberta report), hugging, and dancing – that’s more likely to transmit the (COVID-19) virus,” said Dr Henry in her response to media today. And that’s “regardless of size of particle you’re breathing in at that point”.
Dr Henry emphasized the importance of focusing on reducing those “spaces between us”. Important preventive measures include increased ventilation. she reiterated the experience with food production facilities in the BC Lower Mainland where there were outbreaks early on. “Once the plexiglass barriers were in place and people were wearing masks and there were safe distances between people we stopped the transmission of the virus. That tells me the measures are effective in most situations.”

“A lot of people get sick with this virus in health care settings, in communal accommodation in close quarters,” Dr Henry said today. “A lot of people get sick with this, transmission can be explosive,” she said with reference to the propulsion of air from a patient during certain intensive procedures (such as intubation for being part onto a mechanical respirator) in intensive care.
In situations like that health care workers are “bombarded” and it’s “more difficult to stop the transmission”. That’s why eyes and mouths are covered. “That’s the main reason we’re working so hard so to not be overwhelming the health care system,” said Dr Henry, referring to that requirement of needing personal protective equipment (PPE) as “the burden of the virus in the health care system”.
“Any mistake you make” while taking PPE on or off — especially in close quarters with work mates, where there is “no leeway”, there is “enough virus to run a high risk of being infected”, the provincial health officer explained in her long answer on this topic today. “That’s why we have the protocols in the health care setting. The more virus you have around the more chances of inadvertently becoming infected.”

Precautions that are taken in the community — such as physical distancing, wearing masks, and the use of plexiglass barriers — have worked, says Dr Henry.
Remaining 100% all in:
“Some people shed more virus than others. We can’t tell who that’s going to be,” so it’s best if everyone is playing their part to be “100 percent all in”, as Health Minister Adrian Dix says every time he’s in front of a microphone about COVID-19. He’s refers to adhering with commitment to physical distancing, frequent hand washing, staying home if not feeling well, and wearing a mask if physical distancing cannot be maintained in a close-quarters setting.
Some people may shed a lot of virus even with mild symptoms.” Church services or nightclubs — these are enclosed environments with lots of people where we get lots of (infection)” if there is an opportunity for spread from someone who is carrying COVID-19.
Dr Henry says we “come up with the best of protecting people in those situations”. That includes staying away from others if not feeling well, keeping a safe physical distance, and reducing the number of people in an environment.
Cleaning the physical environment is important:
“We also need to give people the time and space we need to make sure cleaning is done properly,” she said. Many businesses operate with fewer hours (compared to pre-COVID) so they have time for additional cleaning. The premise is the same in schools where time is now given to more thorough cleaning.
Awaiting a vaccine or treatment:

Dr Henry and most public health officials in Canada and the US say that physical distancing and all the other measures that do appear to be effective against the spread of COVID-19 will be in place “until there is an effective treatment or a vaccine”.
This is a comforting thought, though it behooves those of us who are planning our futures to remember that there is still no vaccine for other viral infections such as HIV-AIDS, H1N1 and even the common cold. However, the worldwide health and economic impact of COVID-19 is pushing an unprecedented drive of attention from governments, science and business to aim for ‘herd immunity’ (enough immunity in the population to effectively stop any significant spread).
Meanwhile, we all live in this ‘new normal’, with tight social bubbles, restricted or altered business scenarios, and truncated opportunities in physical social community. In particular, in BC we won’t see the return of large economic drivers (such as large sports events and concerts) until Phase 4 of economic recovery is achieved (possibly not for many years to come).