Wednesday, March 3, 2021 | VICTORIA, BC
by Mary P Brooke, B.Sc., editor | Island Social Trends
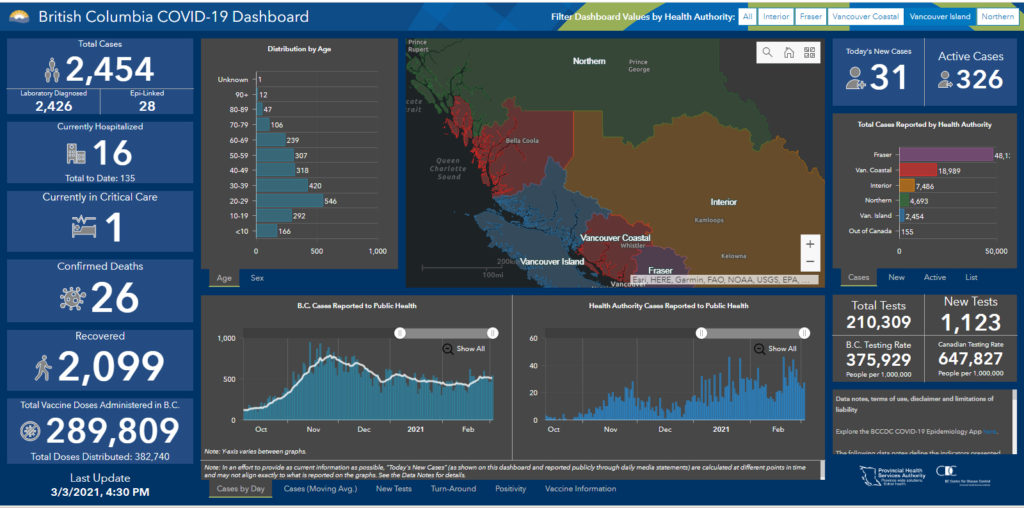
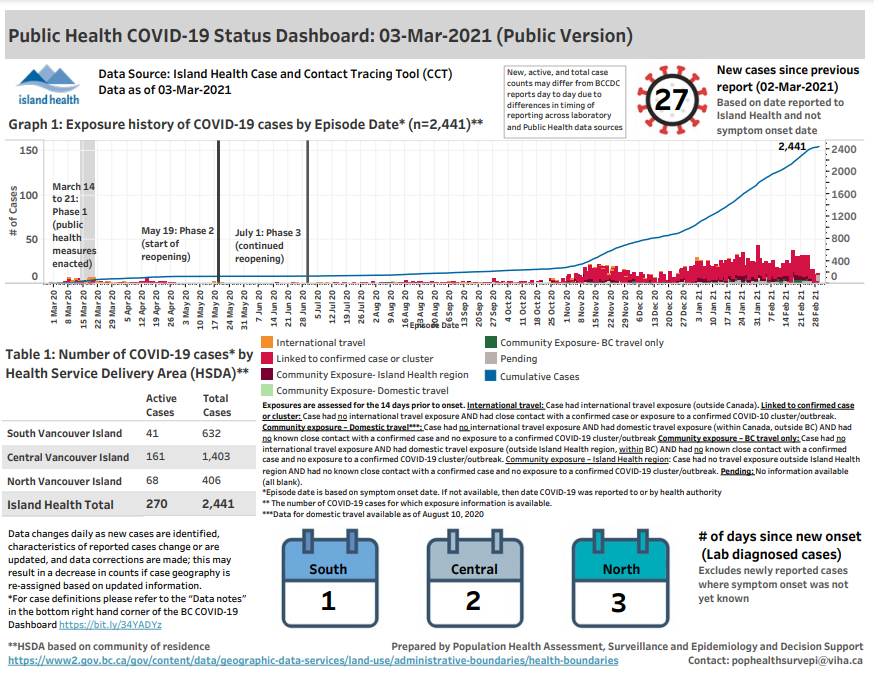
As Vancouver Islanders approach the one-year landmark of dealing with the COVID-19 pandemic (as was declared on March 17, 2020 in BC), here’s where the numbers stand.
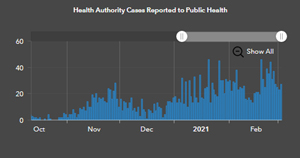
Island Health shows there have been 2,454 cases on the island. That’s about seven cases per day on average, but with data spikes in mid-November 2020 and continually strong daily case counts in January and February of this year which could be said to comprise a ‘second wave’.
Currently there are 326 active cases, with 2,099 people who had tested positive said to be fully recovered.
Island COVID age profile:
By age, the stats for Vancouver Island show the highest number of cases among working-age adults (ages 20 to 59). Here’s the profile to March 3:
- Under age 10: 166
- 10 to 19 years: 292
- 20 to 29 years: 546
- 30 to 39 years: 420
- 40 to 49 years: 318
- 50 to 59 years: 307
- 60 to 69 years: 239
- 70 to 79 years: 106
- 80 to 89 years: 47
- 90+ years: 12
- unknown: 1
Hospitalizations:
A total of 135 people have been hospitalized due to COVID-19 infection, with 16 of those currently in hospital (one currently in ICU).
Of course, hospitalizations are due to cases being more serious, and ICU usually means the person is put onto a ventilator.
Regional distribution:
The central area of Vancouver Island has seen the most cases during the pandemic to date, with 1,403 in that region (161 current) compared to 632 in south Vancouver Island (41 current) and 406 in the north (68 current).
The regional disparity could have to do with lower income living conditions in the central island region.
Deaths:
There have been 26 deaths due to COVID-19 within Island Health. Most of those have been among older people in long-term care (as is the scenario across BC).
Many people dying of COVID in long-term care homes have not been allowed to have people at their bedside, due to public health protocols. The trauma to families as a result of this will linger on.
BC Health knew that congregate settings would be hot spots for infection, based on knowledge of how influenza spreads in those living conditions. To their credit, BC Health brought in a single-site policy for workers to help mitigate transmission and exposure, but maintained ultra-strict rules about visits which has had other impacts.
Vaccinations:
To date, Island Health has received 71,320 doses of mRNA-type COVID-19 vaccines: 46,020 Pfizer and 25,300 Moderna. Of the doses received, so far 39,842 have been administered (10,092 of those as second doses): Pfizer injections at 27,209 (8,261 second doses) and 12,633 Modern injections (1,831).

The AstraZeneca vaccine product is arriving soon in BC, said Provincial Health Officer Dr Bonnie Henry this week. That’s a different type of vaccine (viral vector). Dr Henry says the best vaccine to get is the one you can get (i.e. are offered).
The type of vaccine will depend on where you get your shot (community centre, pharmacy, doctor’s office), your age (older people tend to be given the mRNA type so far), and your geographical location (vaccines requiring less strident shipping temperatures and other conditions).
Islanders have fared better:
Compared to other areas of the province, Vancouver Islanders have fared better in terms of keeping case counts relatively low and seeing generally limited community transmission.
Many thoughts are out there as to why our ‘good luck’ in this regard. Included in those ideas are that we have less dense population, we are inclined by lifestyle choice to go outdoors more and pay attention to healthy choices, a lot of people have jobs which allowed them to work from home, and generally the household sizes (number of people living under one roof) are smaller than in many areas of the lower mainland.
There’s a robustness to the islander mentality (any island anywhere, including historically), where we are quicker to be resilient for a fight. In this case, the fight has been against a microscopic virus.
It might also be said that fewer people on the island have travelled or been in contact with those who have travelled internationally — either by choice or because of low-income.
School exposures:
Currently there is a long list of COVID exposures in schools, in all regions of the island. Overall the school environment has been well-controlled, with exposures being more of a reflection of spread in the community than failures of protocols in the schools themselves, according to Dr Henry.