Thursday June 9, 2022 | VICTORIA, BC
by Mary P Brooke, B.Sc. | Island Social Trends
BC Green Party leader Sonia Furstenau plans to tour the province this summer to meet with health care providers, advocates and patients on what she calls ‘the collapsing public health care system in BC’.
Together with her colleague MLA Adam Olsen, the party leader will travel across BC to meet with health care providers and people struggling to access health care services.
“We will listen to their stories and learn from them. We will bring their voices back to the legislature louder than ever before,” said Furstenau today.

Her party’s criticism is around what the Green’s outline as the government’s lack of preparation for summer climate emergencies, the overload on hospital emergency rooms, understaffing of Urgent and Primary Care clinics (UPCC), continued challenges for people in areas of mental health, nearly one million people in the province without a family doctor, and people dying every day in BC due to poisonous drugs.
Furstenau has released Healthy BC, a summary of the health care announcements and calls that her party has made over the last two years.
Today at a media session, Furstenau was joined by experts who were introduced as non-partisan, including Dr Sanjiv Gandi, pediatric heart surgeon, BC Children’s Hospital; Dr Erika Penner, psychologist and Director of Public Advocacy at BC Psychological Association; and Karen Ward, policy analyst and advocate for drug users.

Preventive health approach:
Furstenau is pushing for an overall rethink of the BC health care system. That includes emphasis on the importance of preventive health initiatives, including access to healthy food and counselling services.
- Dr Gandi opened his remarks by saying “the healthcare system in British Columbia is very good, but far from perfect”. He remarked that government bureaucracies are not clinical care experts, suggesting this leads to efficiency and effectiveness shortfalls.
- Dr Penner suggested that the “burden on family doctors could be lessened if mental health services were treated before they become expensive to treat and before people and loved ones are suffering more”.
- Ward suggested that the solution to reducing toxic drug deaths is to “replace the entire illicit drug supply with regulated substances accessible to all”.
Prevention in schools:
Within the K-12 public education system, the BC Greens Leader (herself a former teacher) hopes to see assurances that students know about healthy food and have access to food.
School districts play an increasingly larger role in meal programs for children and indirectly to their families; this is one of the reasons schools were kept open during the early part of the pandemic in 2020, so that food programs could continue (even shifting staff from other areas to support that goal).
As well, on the mental health side of things, Furstenau feels there should be more funding for and/or availability to counsellors (and notes that the Counsellors of BC want to be regulated health care providers, as a way to maintain standards).
Some school districts (like SD62 in the west shore of Greater Victoria) have tried to find creative ways to support students’ mental wellness needs through other programs, precisely to cap off problems before they emerge in a more complex way that would require counsellors. They maintain a robust Healthy Schools, Healthy People program.
Access to primary care:
All the speakers agreed that access to a primary care physician is fundamental to overall better health care service to the population as well as supporting better overall function of the health care system.
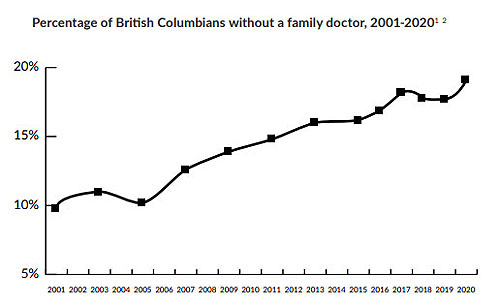
Furstenau quoted from a letter dated June 2000 from then-NDP health minister Mike Farnworth, articulating quite well the looming problem of the family doctor shortage in BC. Essentially, the system of family doctors running their own businesses — and then quitting due to overhead costs and/or retiring without finding a replacement — was articulated over 20 years ago.
Now over 100,000 people in BC don’t have a family doctor, as the lifestyle preferences and retirement of doctors has become an acute problem.
The NDP government and Health Minister Adrian Dix have rolled out many Urgent and Primary Care Care Centres (UPCCs) in BC since forming government in 2017. But the UPCCs seem to be chronically under-staffed, even though — as Dix himself has mentioned this year — that BC is graduating more doctors from medical school than ever before.
Seeking more through the Canada Health Transfer:
Furnstenau is calling for a health care plan and not just throwing more dollars toward the system without a clear new or revised approach to the current system. She notes that Premier Horgan — as chair of the Council of the Federation (COF) — has essentially said ‘send us the money first, then we’ll build a plan’ (referring to provinces needing larger budgets in order to deliver health care in their jurisdictions).
Orientation toward prevention and dealing with people’s health care problems before they become larger and more complex (and therefore more costly to address) is the direction that the BC Greens (and today’s non-partisan speakers) propose.
Dealing with the cost of health care administration is part of the challenge, said Furstenau as well as one of the medical doctors.

The BC Greens want to see an update the family physician payment model to incentivize family practice and properly support the work of doctors. The NDP government has already acknowledged the need for that. Any change there would require negotiations with the Doctors of BC, which of course to do so responsibly, the government would need to know the dollars are there (hence the Canada Health Transfer increase goal).
Next month Premier Horgan will chair a COF meeting of the premiers, in Victoria. Horgan has discussed the Canada Health Transfer issue with Prime Minister Justin Trudeau many times.
Illicit drug supply:
The BC Greens see part of the toxic drug overdose problem (six deaths per day in BC) as being addressed by replacing the range of illicit drugs with regulated substances that are accessible. This certainly does required getting past any blame or stigma about substance use.
The BC government approach to date (currently under the wing of Sheila Malcolmson, Minister of Mental Health and Addictions) has been to address addiction and overdoses on an emergency basis (including administration of Naloxone by paramedics), and — if the patient is willing — then accept treatment to get beyond their addiction. The BC Government has made significant investments in addiction recovery ‘beds’, i.e. embedding addiction recovery within the health care system. Some of that does include wrap-around supports like transitional housing and job-seeking support, but it would make sense to try and stem the socioeconomic causes before an acute medical problem occurs.
===== RELATED:
Premier Horgan still pitching for Canada Health Transfer increase (April 21, 2022)
Trudeau & Freeland: Planning and clarity needed for federal funding into health-care (April 11, 2022)
Affordability, health-care & climate impacts top list of Canadian concerns (February 4, 2022)
Premiers push for higher federal health-care funding (February 4, 2022)
NDP 2022: pushing for economic stability & health equity (January 31, 2022)
Worker drug-poisoning prevention led by Vancouver Island construction industry (January 13, 2022)
Trudeau & Horgan: Omicron, Canada Health Transfer, disaster response (January 4, 2022)