Thursday April 4, 2024 | VICTORIA, BC
by Mary P Brooke | Island Social Trends
Health Minister Adrian Dix has proudly stated in recent days that BC has 708 ‘net-new’ family doctors (some have left, more have arrived or switched into the new longitudinal model).
‘Longitudinal’ doctors are physicians taking patients for care over the longer term without the increasingly outdated fee-for-service model. That could be in private practice or at clinics.
Longitudinal model:
The longitudinal family physician (LFP) payment model gives doctors the option to not use the fee-for-service model; that model which saw doctors operate their practice as a small business (covering all their own expenses including office and staffing), paid them a flat rate of around $30 per patient visit, whether they were treating a simple ailment or a complex chronic health condition.
The LFP model, which was launched on Feb. 1, 2023, compensates doctors for the number of patients they see, the complexity of their needs, and time spent on other necessary tasks like reviewing lab results, consulting with other medical professionals, updating patient lists and clinical administrative work.
Among other points, the BC Government pitches that the longitudinal care model is suitable for doctors who “value the time spent with patients”. The model is setup to “acknowledge the value of indirect care and clinical administrative services”.
Net-new profile:
BC Health points out that Vancouver and Fraser Health had strong increases but that Island Health had the most significant lift at 179 more family doctors this year compared to last year – an increase of about 20%.
The table below has been provided by BC Health this week:
| Longitudinal Family Physicians, by Health Authority, April 1 to December 31, 2022/2023 and 2023/2024 | |||
| Health Authority | 2022/2023 | 2023/2024 | Difference |
| FHA [Fraser Health] | 1,308 | 1,440 | 132 |
| IHA [Interior Health] | 766 | 904 | 138 |
| NHA [Northern Health] | 246 | 281 | 35 |
| VCHA [Vancouver Coastal Health] | 1,179 | 1,390 | 211 |
| VIHA [Island Health] | 775 | 954 | 179 |
| Unknown HA | 15 | 28 | 13 |
| Total | 4,289 | 4,997 | 708 |
Family doctor’s role:
In the BC health care system the point of entry for any further care is usually through a family doctor (general practitioner / GP). If a person’s health care needs requirement lab tests or scans, or the care of a specialist, all that must start with authorization from a family doctor.
The signature of a family doctor is also required for various types of paperwork including insurance and disability-related matters.
Without a family doctor in BC:
If you don’t have a family doctor, you can visit a walk-in clinic. HealthLink B.C., a provincial telehealth service, has a search tool that lets you find listings for health services, including walk-in clinics, hospitals and emergency departments. You can also use Medimap to find a walk-in clinic near your area.
Last year, the province reported there were 895,000 people in B.C. without a family doctor, compared to 980,000 people in B.C. were without a family doctor three years ago. This decrease in the number of people seeking a family doctor is seen as significant given that there has been an overall population surge of 300,000 over the past three years.
Health vs wellness:
BC Green Leader Sonia Furstenau says that the health-care system in BC requires more attention to preventive care as well as increasing the number of family doctors. Last month she mentioned the impact of wildfire smoke on people in communities. She said the “fossil fuel industry is delivering some of the greatest public harms”.
Taking take of disease versus well-being is a BC Green direction. Furstenau says she hears from health professionals and advocates that people need “quick access to primary and preventative care”. She claims that teams of doctors are “hitting resistance at every front from the Ministry of Health” in terms of getting health-care clinic rolling. Minister Dix has rolled out several new Urgent Primary Care Centres (UPCC) across BC in recent years but perhaps it’s not enough. She does support team-based care, which is the thrust of the government’s UPCC’s.
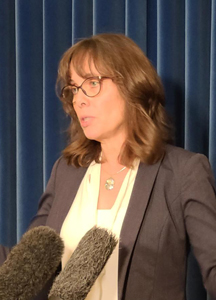
She gave the example of women not getting mammograms in a timely fashion. Though it should be noted that BC Health just launched their at-home HPV testing program to take the load off in-office appointments for PAP tests for cervical cancer. So there are some innovative steps being taken in BC, in some cases well ahead of what other provinces are doing.
“Investments in both public health and primary care that are absolutely necessary if we’re going to turn around the very dire impacts that we’re seeing on acute care right now,” said Furstenau in a media session on March 14.

“The gaps that have been widened in the last seven years are being filled by private, for-profit companies that are delivering health-care for an additional cost. We start to see a greater and growing inequality exacerbated by people who can pay to get access to timely primary care and people who are standing in line at 5:30 in the morning who are trying to get into their primary care centre, They find out day after day they are not going to get access to that primary care,” said Furstenau.
The shortage of immediate access to primary care seems to have become ‘the new normal’ in BC. In Greater Victoria, up until the early 2000’s it was possible to drop-in to a local clinic without an appointment and be seen within an hour or two.
“I don’t accept our current state of affairs as the ‘new normal’. Everyone deserves better – better outcomes for things that matter most to you,” says BC Green candidate Camille Currie, who makes health care the focus of her campaigns (first in the 2023 by-election in Langford-Juan de Fuca and now in Esquimalt-Colwood in the upcoming 2024 provincial election.
Problems down the road:
It is generally accepted that when minor health issues are not readily dealt with that problems can grow in larger health issues for patients. This is a harbinger of an even more significant load on the health care system in the years ahead.
Compounding the health-care patient profile in the years ahead is that the population of people over 65 is increasing; advancing age is usually associated with greater need for attention to health-related care.
The overall population has ballooned in recent years (up by 300,000 in the last three years).
The workforce available to the health-care system is still strained; BC is looking to skilled immigrants to fill many of the roles that will be opening up.
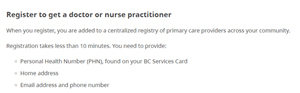
BC Health Connect Registry offers no guarantees:
The BC Government has a BC Health Connect Registry where a person who is in search of a family doctor or nurse practitioner can enter their name and basic details such as age, location, and how long they have been without a family doctor.
However, that seems not really enough to go on for doctors who are seeking or accepting new patients. For example, a patient’s age is a very broad indicator of what their health condition might be (e.g. smoker vs non-smoker, active vs sedentary, already with a chronic illness, etc.).
You can register yourself and your family members. You can also register on behalf of a person in your care, for example, you may be a healthcare provider or social worker.
If you’re already on a waitlist at your local clinic, you do not need to register. Primary care provider waitlists at all clinics and community health services in B.C. are transitioning to the Health Connect Registry.
The BC Health Connect Registry says that you will be contacted directly about your registration. You will maintain your original waitlist registration date.
That is no guarantee that a person will be invited to meet with a family doctor. BC Health Minister Dix said last year that seniors would likely be prioritized but later retracted that, saying that doctors will want to choose their own clients and build out a clientele profile that suits their career interests. As older people generally have more complex health issues, it’s possible that especially new doctors wouldn’t want to fill their ‘bingo card’ entirely and right from the start with patients with a range of complex and/or chronic needs.
Team-based care:
The team-based approach to patient care — that sees groups of doctors work with nurse practitioners, pharmacists, and social workers — can create a high-functioning primary care system.

Urgent Primary Care Centres have been opened in various locations in BC under the current NDP government since 2017.
Health Minister Adrian Dix:
Adrian Dix has been the health minister since 2017, first appointed by John Horgan and kept on by David Eby when he became premier at the end of 2022.
He has attempted to deal with the breadth of issues of managing health-care in BC from dealing with the personnel shortages to activating capital expansions for clinics, hospitals and specialized care services like cancer services.
Dix has expressed pride in having been a part of one of the most successful COVID immunization rollouts in North America and overall management of the pandemic where schools stayed open and surgeries (first postponed) were caught up.
===== RELATED:
- HEALTH NEWS SECTION (2018 to present)
- National Caregiver Day: recognizing their work & commitment (April 2, 2024)
- Westshore Urgent Primary Care shifts to appointment booking by phone (March 18, 2024)
- BC Greens seek fire department gear upgrade for better health protection (March 15, 2024)
- Jan 2024 respiratory season update emphasizes vaccination (January 10, 2024)
- HPV tests at home may help boost patient-doctor attachment (January 9, 2024)
- Island Health Dec 2023 holiday season clinic hours (December 21, 2023)