Sunday November 27, 2022 | VANCOUVER, BC
by Mary P Brooke | Island Social Trends
More family doctors will be available to take patients and treat people in BC as the Province expands a program that trains internationally educated doctors, so they can get licensed to practise in British Columbia.

This livestreamed announcement was made at 1:30 pm today, Sunday November 27, in Vancouver, by Premier David Eby and Health Minister Adrian Dix.
Practice Ready Assessment program:
Expansion of the Practice Ready Assessment (PRA-BC) program will triple from 32 seats to 96 seats by March 2024.
The PRA-BC program is a pathway for internationally educated family doctors to be licensed to work in BC. “Expansion of this program — particularly in primary care — is an important change and will get dramatically bigger over time,” said Dix today.
Physicians who qualify under this program will perform as Associate Physicians under the supervision of a BC-licensed doctor, explained Eby.
BC needs to “get more (doctors) off the sidelines (and into practice),” the Premier said today.
Underlying population changes:
“The pandemic has exposed underlying challenges and added new strains to our public health-care system, and too many British Columbians are struggling to find a family doctor,” said Premier Eby.
“Meanwhile, family doctors trained outside of Canada aren’t able to practise family medicine, because they lack a pathway to be licensed here. We need to fix this,” said Eby.
“That’s why we’re taking action to help get more internationally trained doctors off the sidelines and into communities where they are so desperately needed.”
USA-trained doctors can come right away:
Minister Dix outlined that doctors trained in the United States (and have three years experience) and come here right away to work here, highlighting areas of pediatrics, emergency rooms, and internal medicine.
“We welcome this component of addressing a need” within what Dix described as a “larger action plan”.
The greater facility of accepting USA-trained doctors into the BC system highlights the overall challenge of bringing in internationally-educated doctors, nurses and other health care professionals, i.e. the ability to communicate fluently in English. Rarely is the language component mentioned, but that’s been fundamental to the challenge of accepting internationally-trained doctors up until now.
Doctor shortage:
Adrian Dix has been the Health Minister in the BC NDP government since the beginning in 2017. He was the opposition Health Critic before that. He notes that in 2003 there were 300,000 people in BC without a family doctor, a tally that by 2017 had tripled to 900,000.
Around 2015-2016 the previous government had announced or promised the addition of more doctors in BC, but nothing materialized.
Many family doctors (general practitioners) have been retiring (completing their career-long practice) in the last five to 10 years, which has been a notable component of the GP shortage. Another component is the overhead cost of running a private family practice as a small business.
Two doctors spoke today:
Dr. Ramneek Dosanjh, president, Doctors of BC, said she is pleased that the provincial government is making it easier for more US and internationally trained family doctors to practice in BC.

“It Is something Doctors of BC has long advocated for. Given the challenges in our primary care system and the number of patients without a family doctor, these changes will greatly benefit British Columbians,” she said today.
Dr. Ehab Fadhel, a family doctor in Victoria who completed the Practice Ready Assessment program in 2022, said the Practice Ready Assessment program fully prepared him to be a family doctor at the Arbutus Family Medicine clinic in Victoria.

“After training in Qatar and in the United States, I am proud to care for my patients in my new community and I am happy that more physicians will be able to live and build a rewarding career in BC like I am,” said Dr Fadhel.
Adjusting to new realities:
On top of the retirement and small business factors, the challenge for maintaining the number of GP’s has been exacerbated by the per-patient-visit flat fee payment system. That billing system has only recently (in summer/fall 2022) seen the start of adaptation to the realities of one-on-one patient care by GPs.
Some patients have more complex needs — particularly seniors (in this province which has a very high number of seniors) and people with chronic conditions. As well, the need for translation services in patient care have not only slowed down service delivery but potentially compromised patient privacy and confidentiality.
Today Dix said about “seven, eight or nine” steps have been taken, so far, in adjusting to the new realities of delivering health care in BC. He noted the collaborations with the Doctors of BC, increasing nursing spaces, improving safety and security in health care facilities, and increasing the number of health care workers.
Dix described a “net new” 38,000 health care workers as “that’s impressive”, adding: “We need to do that again in the next five years coming up, and in the five years after that.”
Dix said that “breaking down barriers for internationally trained nurses” has been significant.
Urban vs rural, including mental health:
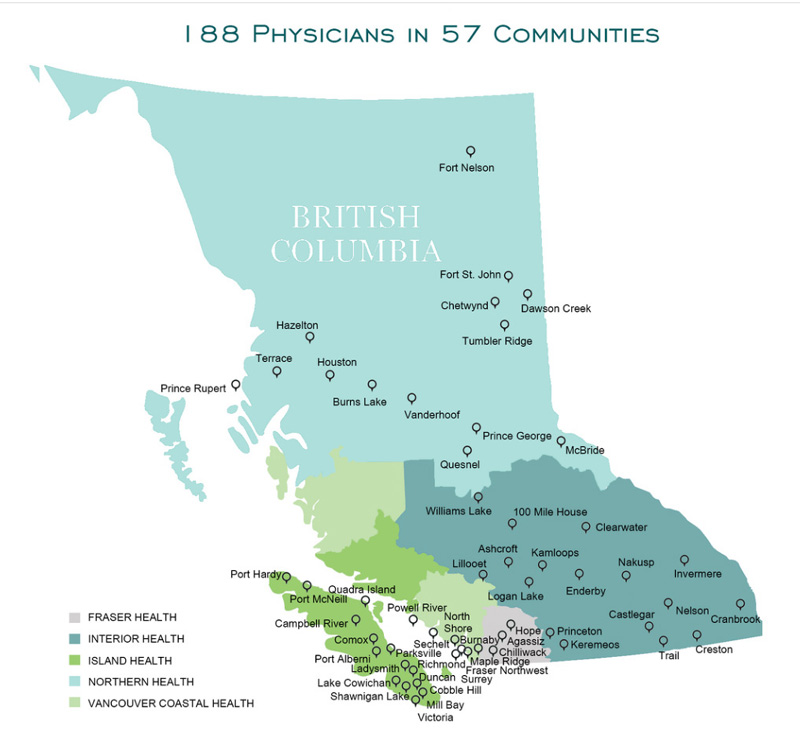
After successfully completing an assessment, physicians receive a provisional license and are positioned for a three-year return of service in a community of identified need.
Half of the incoming physicians in the Practice Ready Assessment program go first to rural and remote areas, Dix explained today.
In Greater Victoria where the population has been increasing in the age 75+ category, there have been “older family doctors in those communities”, and therefore some attention by Minister Dix to addressing shortages there.
The attention to filling the need for doctors in pediatrics, ER, and internal medicine generally addresses shortages in hospital and acute care settings.
Most of the increases in GPs have been in the area of family medicine so far, which Dix says includes “mental health and addictions” as part of being “at the core of primary care”. He notes that BC has seen 1,200 new workers in mental health and addictions and counselling, under his watch.
There was no stated allotment for one health authority over another. BC has five regional health authorities plan and coordinate the delivery of provincial programs and specialized services, and a First Nations Health Authority.
Urgent Primary Care Centres:
Many Urgent Primary Care Centres (UPCCs) have been opened in BC while Dix has been Health Minister, but the UPCCs were not really mentioned today. UPCC’s have met with moderate success, in that it’s been a challenge to find and retain doctors who want to work in that model which is salary-based and relies on a network of allied health professionals in the same venue.

UPCCs are mostly in urban settings, including one in the west shore (Langford), another in James Bay (downtown Victoria) and one in Esquimalt, and others in areas of the Vancouver/Lower Mainland area.
Today Premier Eby said the incoming American doctors would be helpful in “community settings for adults and pediatrics” and in UPCCs. Some new ones will be arriving in January 2023, he said, adding that “every step we take gets us closer to our goal”.
Collaborative approach:
“None of these changes would be possible without the collaboration and support of the Doctors of BC,” said Dix, several times during today’s livestreamed media session.
“Patients and doctors need all the help we can get,” said Dix, adding that there are doctors “dreaming of coming here”.
“By tripling the number of seats over the next 16 months under the Practice Ready Assessment program, providing a new pathway for international medical graduates to work as associate physicians, and removing barriers for doctors from the United States to work in B.C., we are delivering in our commitment to patients and building strong team-based care for all British Columbians,” said Adrian Dix, Minister of Health.

Program details:
International medical graduates (IMGs) who are not eligible for full or provisional licensure in BC may be eligible for a new associate physician class of restricted registration with the College of Physicians and Surgeons of BC (CPSBC). This will allow them to care for patients under the direction and supervision of an attending physician within a health authority acute-care setting. This is part of government’s work to recruit more health professionals and provide immediate solutions for people who need to access health services. The Ministry of Health is also working with the CPSBC to expand the new class, so associate physicians can work in community-based primary care settings over the coming months.
The Province is working with the Royal College of Physicians and Surgeons of Canada and the College of Family Physicians of Canada to allow IMGs to start the accreditation process before they arrive in BC. Doctors interested in moving to BC will have increased certainty of being able to practise when they arrive, so they can support doctors and begin treating patients.
The College of Physicians and Surgeons of BC will prepare bylaw changes to allow doctors trained in the U.S. for three years to practise medicine in community settings, such as urgent and primary care centres, community clinics and family practices. These doctors will be able to care for adult and pediatric patients, as well as provide emergency and urgent care. The bylaw changes will be implemented in the coming weeks, with the intent of allowing these doctors to practise medicine in BC communities by January 2023.
These actions are part of BC’s Health Human Resources Strategy, which was announced on September 29, 2022. The strategy supports patients by ensuring they get the health services they need and are cared for by a healthy workforce. It focuses on 70 key actions to recruit, train and retain health-care workers, while redesigning the health-care system to foster workplace satisfaction and innovation.
First 100 days:
Today’s Sunday news session comes on the heels of several announcements by Premier Eby (including Sunday last weekend), as part of his stated political goal to show a lot of action and new approaches in his first 100 days in office.
So far Eby has covered crime (funding the hiring of more police officers), housing (launching a standalone housing ministry and opening up pre-2010 strata condos for rental), affordability (with two cost of living credits), and health care (including restoring hospital support workers to in-house positions).
Eby was sworn in November 18, 2022 in Vancouver and will announce his new cabinet on December 7, 2022 in Victoria.
===== LINKS (BC Government):
Practice Ready Assessment: https://www.prabc.ca/
Associate physician class of registration: https://www.cpsbc.ca/registrants/current-registrants/registration-and-licensing/defined-scope/associate.
IMGs seeking information about associate physician employment opportunities are encouraged to contact Health Match BC: https://www.healthmatchbc.org/About-Us/Contact-Us/Contact-Us-(Physicians)
BC’s Health Human Resource Strategy: https://news.gov.bc.ca/releases/2022HLTH0059-001464
===== ABOUT ISLAND SOCIAL TRENDS:
Island Social Trends is a professional news portal at islandsocialtrends.ca . Fully online since mid-2020, Island Social Trends emerged from the extensive regional groundwork of previous print publications in the west shore: MapleLine Magazine (2008-2010), Sooke Voice News (2011-2013), and West Shore Voice News (2014-2020).
Since 2008, journalist and editor Mary P Brooke has taken a socioeconomic lens to the news of the west shore and south Vancouver Island region, including BC provincial news, and national news impacts.
===== Island Social Trends ARCHIVES: