
Tuesday November 3, 2020 | VICTORIA, BC [Updated 12:30 am November 4 2020]
by Mary P Brooke, B.Sc., editor | Island Social Trends
‘Staying Apart to Stay Safe – The Impact of Visit Restrictions on Long-Term Care and Assisted Living Survey’ results were released today by BC Seniors Advocate Isobel Mackenzie in a livestreamed media teleconference from Victoria.
Over 13,000 people contributed to the survey — mostly family members of people in long-term care and residents (as well as some workers in the sector), over a period of just over four weeks (August 26 through September 30, 2020).
Overall, family members expressed wanting more time with their loved ones in long-term care — not only to provide essential support such as feeding and personal grooming but to provide social and emotional support. That support is key for the person in care but also connects back to the well being of loved ones in the broader family who are not left with possibly years of dismay over missed opportunities with loved one in their final years, months or days.
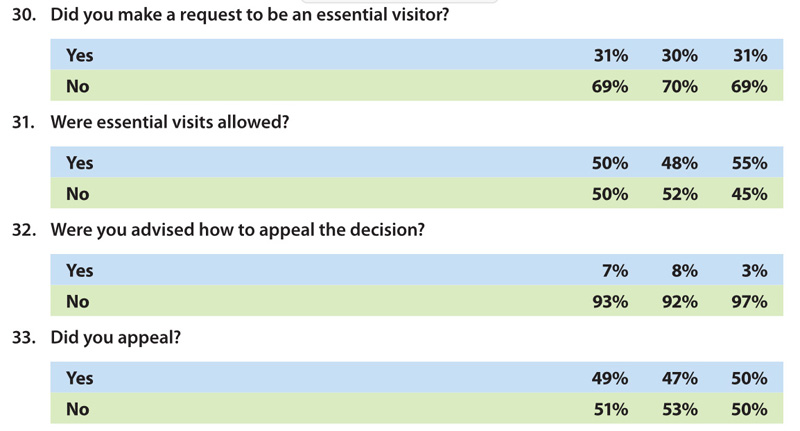
The survey results show how half of the people who requested visits with their loved ones in long-term care during the pandemic were denied that request. Only seven percent were guided on how to appeal, though 49 percent did appeal.
Quality of life, quality of visits:
Mackenzie highlighted that quality of life in the years at end-of-life is what matters more for most of these survey respondents than the extension of life in a state of enforced isolation. She even clarified that some residents said they would rather get (and even die) from COVID-19 than be permanently or artificially separated from the loved ones who would otherwise come to visit them.
She said that most if not all impacted families (among the survey participants) said they are in agreement with wearing a mask, getting tested for COVID before visiting, and scheduling of visits. The key thing was to have access and that time spent with an aging parent or grandparent be in their private room (not in common areas with supervision, or outdoors). That would be produce some semblance of a ‘home’ environment for the visit.
Essential care partner, private room visits:

Today Isobel Mackenzie said there has been “no record of transmission (of COVID) from a visitor”.
In that context, she emphasized how a family member who comes to visit an elder in long-term care is also an “essential care partner”. Their presence can be of help to “staff that have been overburdened”.
As part of a wholesome visit: “We need to communicate with absolute clarity to long-term care homes that visits need to happen in a private room,” the BC Advocate for Seniors told media today.
Recommendations to improve current conditions:
Three recommendations delivered in the report summed up the needed direction that the findings indicate:
- All residents need the opportunity to identify an essential care partner who can visit frequently and provide those supports and services that are essential to the health, physical and emotional well-being of the resident.
- In addition to the essential care partner, residents need social visitors, and the number allowed needs to balance the risk of COVID-19 with the risks to resident health, happiness and quality of life that results from long-term family separation.
- The voice of residents and their family members must be embedded in decisions on how we shape our long-term care and assisted living system in British Columbia going forward. The Ministry of Health needs to collaborate with the Office of the Seniors Advocate to create a provincial association of long-term care and assisted living resident and family councils.
What COVID has taught us:
“The pandemic has taught us many things beyond the basic science of infectious diseases. We have learned much about ourselves and each other as we unite to make it through this pandemic together,” Mackenzie said today.

“These troubled times have made us reflect on what we value in life and we have found that, for many of us, the top priority is the time we spend with our family and loved ones,” she stated in the written report and reinforced in her one-hour media session that was livestreamed on the BC government video channel.
“With compassion and kindness to temper clinical decisions around safety, we can thoughtfully respond to the needs of our seniors and their families. Finding the right balance will be challenging but it is the right thing to do as we seek to bring joy, comfort and an enhanced quality of life to British Columbia’s seniors.”
Yes, there is some risk:

Mackenzie admits there would be some level of COVID-risk to have people visiting in care homes.
But she quickly added that there is never zero risk in anything in life, and highlighted there is risk in other areas of well-managed community scenarios at this time including children and teachers in schools, children and drivers on school buses, and both workers and customers in grocery stores.
“We’re learning how to live with this virus,” Isobel Mackenzie said today. She noted how long-term care homes with government support got personal protective equipment (PPE) and staffing in place. This phase of adapting for meaningful and frequent-enough family visits can be achieved as well, she believes.
Timeline and regions:
“If not now, then when,” said Mackenzie rhetorically today, as to the necessity to act on the recommendations right away. She outlined how we are now nine months into the pandemic and no one knows how long it will be until there is a vaccine or other form of social normalization again.
BC Centre for Disease Control statistics show there have been no COVID outbreaks in long-term care on Vancouver Island, and today Isobel Mackenzie affirmed that the most significant spread of COVID is in the Fraser Health region in the lower mainland area. She feels it would be appropriate to have a regional approach to various aspects of COVID response by public health.
Sources of support:

The survey respondents contributed the details and momentum to enable the path forward for allowing supportive visits in long-term care.
Mackenzie also thanked the Provincial Health Officer (Dr Bonnie Henry) and the BC Government (with Health Minister Adrian Dix as Minister of Health) for their swift and unquestioning support of her initial requests for adequate PPE in long term care, and ultimately what was a government instruction to long-term care that all workers be single-site (not working at more than one site).

The effort and dollars that went to this mobilization of resources “quickly and without argument” was acknowledged by the seniors care advocate.
“You have my profound gratitude,” said Isobel Mackenzie through these words to Dr Henry and Adrian Dix and their teams.
As well, during the recent provincial election campaign, BC NDP Leader (now premier-elect) John Horgan promised private rooms for all long-term care facilities, over time. He’d been listening to the science (COVID is more easily spread in communal living environments) and to the expressed need for social support and private visits.
Download the report:
The 38-page November 2020 report and survey findings are available online on the BC Seniors Advocate website.
Mackenzie said today that the report was prepared in record time, implying the urgent need for the proposed changes in the management of long-term care with regard to visits.
The report includes statistics, personal stories (that were heard during the survey process), and the recommendations along with background discussion.
About Isobel Mackenzie:
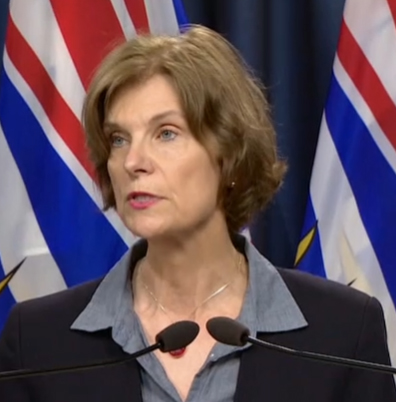
BC Seniors Advocate Isobel Mackenzie was appointed to her position by the BC Government in March 2014, becoming the first to hold that role within (but independent from) government across Canada. She has over 20 years of experience working with seniors in home care, licensed care, community services and volunteer services. Prior to the BC Adovate role she led BC’s largest not-for-profit agency, serving over 6,000 seniors annually.
This year, Mackenzie began expressing concerns about the social and emotional health needs of seniors and their families as relates to visits in long-term care during the COVID pandemic back in April. That was about one month after the BC government declared a public health emergency as a result of the global COVID pandemic (March 17) followed by declaring a state of emergency in BC (March 18).

===== About the writer: Island Social Trends editor Mary P Brooke holds a B.Sc. in health science, with a strong community education component and a second major in sociology. This publication explores the many aspects of societal well-being.




