Saturday November 30, 2024 / 7:12 pm | VICTORIA, BC [Updated 9:26 pm]
News analysis by Mary P Brooke, B.Sc. | Island Social Trends
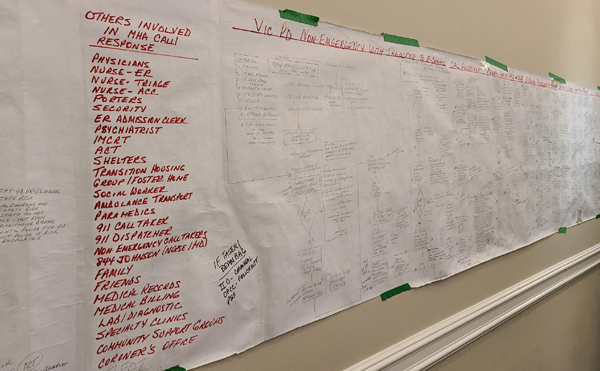
Working with at least two older systems in need of revision — policing and hospital-based health care — people who fall into the jaws of how mental health-related incidents are handled in BC have been the victims.
In comes Dr Eileen Pepler who has a vision to develop effective systems of care for people both before (if ever) they meet up with the policing system in a mental health incident and if they in fact become enmeshed with a societal-system response to their situation.
She wants to ensure that society and government begin to see mental health services as a right not a privilege.
Medical not criminal:
Stepping back for a moment … mental health challenges are a medical problem, not a criminal problem. That has been well-established through the lens of health, social and legal.
Treating a ‘mental health incident’ as a problem requiring a police (enforcement) response is a throwback to a time when society was so rigid that people either fit or they did not, when the safety of the people around the ill person took extreme precedence over the well-being of the struggling individual.

People can suffer from mental illness for entirely physical metabolic reasons and/or as a result of psychological or physical trauma. When their behaviour acts out on that, the current response in the day-to-day realm is to see the behaviour as a threat — either to others or to the person themselves.
Some of this has been recognized, as seen in recent pairing of nurses with police for heading out on ‘mental health calls’. That is still a law enforcement visit, with the nurse along to possibly defuse but more so because only the nurse will have access to the person’s medical file.

The cost that can spiral out of control from just one mental health care is quite staggering.
Approaching the provincial government:
This is the tip of the iceberg as to what Pepler presented to a room full of influential women in business and community this week. She will have their support as she heads into a what she hopes will be a meeting with Premier David Eby and the new BC Health Minister Josie Osborne and possibly also Parliamentary Secretary for Mental Health and Addictions, Amna Shah.
Having the entire health file under one Ministry may help get adequate and appropriate funding for mental health programs and supports, says Pepler.

New BC cabinet ministers were only appointed less than two weeks ago. Pepler is one of many sector representatives who will be seeking the ear of new cabinet ministers and parliamentary secretaries who have responsibility for key areas of society.
“They can’t afford to fail this time,” says Pepler about Eby and his new 47-seat slim majority government. She hopes to provide the health ministry with the information they need in order to steer mental health approaches toward success. ” I want them to really understand what is at stake,” Pepler told her audience of business and professional women leaders yesterday.
Mental health approaches over the past seven years:
For the previous seven years Health was one ministry (under Adrian Dix) and Mental Health and Addictions was handled in a separate ministry under different ministers over the years. Most people, agencies, medical professionals and leaders in government would likely agree that not enough has been done about mental health-related issues in the past seven years.

The police act is under revision thanks to the NDP government, some community health clinics have taken a same-day approach to seeing people in need (a clinic like that was brought to the west shore by now former MLA Mitzi Dean), and some school districts have tried their hand at various programs (e.g. School District 62 has tried to expand out with peer support instead of adding more clinical counsellors).
But otherwise people are falling between the cracks across society with a varying range of mental health challenges. There is little to no public education about the role of natural healthy food in the maintenance of good health. Of course skyrocketing grocery prices don’t help in that regard. Politics is a large part of that. Recently the federal NDP brought forward a bill to help foster more competition in the grocery store sector.
A key aspect of mental well-being is a sense of belonging as well as resilience. In a fast-changing society and difficult economy, but of those goals for well-being are often seriously challenged. As Pepler points out, people who have the money to get help will find it, while most of the others will not.
For Pepler it’s about breaking silos as a way to finding and achieving sustainable mental health solutions. She points out that mental health services are not part of the Canada Health Act. That is part of how underfunding happens.
Mental health funding:
In BC, the data about mental health funding in the 2024-2025 budget is insufficient (also in Quebec); this could be because the delivery of mental health services is spread out through various channels. In other provinces available data shows a 7.5% mental health funding component in Nunavut at 10% (the highest of the provinces and territories), with 7,5% in Saskatchewan, 6.9% in PEI, 6.4% in Yukon, New Brunswick with 6% and Ontario at 5.9%.
Defining exactly what ‘mental health services’ really are seems to be part of the challenge. Is is programs, or time with a psychologist or counsellor, or get direct addictions care? Does it mean guiding people to stable employment or finding a place to live? Does it mean dealing with active or lingering impacts of abuse? The range of causes for mental distress is vast.
Amplifying the mental health crisis is the use of drugs and illicit substances which are oftentimes addictive and or toxic. Deaths from substance use (toxic through illegal impacts like fentanyl, or otherwise) are a related problem but which comes with its own challenges. Figuring out why people want to escape through the use of drugs is about getting to root causes. And that won’t be solved during a ‘mental health check’ by police or even direct intervention to deal with the physical aspects of addiction.
Pandemic fallout:
Pepler does point out that the incidence of mental health challenges has become worse since the pandemic. During the years 2020 and 2021 people were told to socially and physically isolate. This damaged family bonds and personal relationships. Young adults in particular couldn’t get their lives off to a normal active start. The impacts have lingered if not festered since then.
According to a 2024 report called The State of Mental Health (as released by the Canadian Mental Health Association) 10 million Canadians (about one in four) report ‘poor’ or ‘fair’ mental health. Apparently that’s three times more compared to pre-pandemic.
About Dr Pepler:
Dr Eileen Pepler is the principal and managing partner at the Victoria-based Pepler Group which aims for ‘smart systems for better outcomes’.
She has more than 25 years of management consulting, health and social policy planning, research, sales, marketing, consulting and academic experience.
Pepler is big on data and measurement. In the Greater Victoria area she has helped the Township of Esquimalt with community health needs assessment that helped them to develop a strategy to assess the health care needs of their local community which led to getting two health clinics (one of which is the Esquimalt Island Health Urgent Primary Care Centre).
She is pleased that her work helped inform and influence change in the 9-1-1 emergency call response system that was fleshed out post-pandemic. Incoming calls have long been categorized as responding to fire, ambulance or police. Now mental health is added to that, thanks to decisions taken by Victoria Police and Island Health.
Vast project:
While the scope of entwining mental health within the provincial health-care system seems like such a massive problem with no one place to start, Dr Pepler hopes to tackle the starting gate with meetings with the provincial government soon.
“We can’t keep using the health care system as a dart board,” says Pepler. She hopes to bring some focus to the matter where it has to do with mental health.
Anyone who would like to support Dr Pepler’s work can reach out to her at Pepler Group.
===== RELATED:
- Westshore Mental Health and Substance Use Service Hub has opened in Colwood (August 29, 2024)
- New West Shore RCMP unit will respond to mental health calls (July 17, 2023)
- Esquimalt UPCC opens at permanent new location (December 6, 2021)
- NEWS SECTIONS: HEALTH | WELLNESS & PREVENTION