Saturday December 26, 2020 | VICTORIA, BC
Editorial Analysis by Mary P Brooke, B.Sc., editor | Island Social Trends
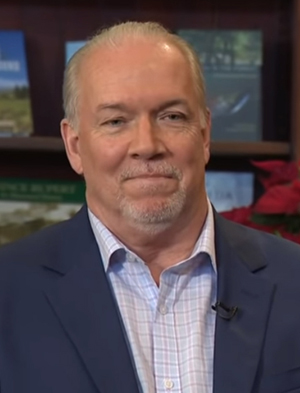
Some things could have been done better, but overall BC has fared well through the pandemic. That was a leading point of Premier John Horgan’s answers to year-end questions in a Global TV year-end interview (taped ahead of Christmas) first aired on Christmas Day, and again on Boxing Day, as this pandemic-year 2020 comes to a close.
At the top of Horgan’s list of things that might have been taken on not-so-stridently was the complete shutdown of surgeries in the first wave of COVID-19 BC, said Horgan. “There wasn’t the surge that we anticipated,” he readily admitted in his interview with Global News reporter Richard Zussman.
“The second wave has been profound on all of us,” said Premier Horgan, noting that over 700 people have lost their lives to COVID-19 in BC (specifically 808 deaths as of December 24 | BC CDC stats). Incidentally, compare that death tally to 314 traffic fatalities across BC in one year (2018) (ICBC stats) and 1,548 deaths due to opioid overdoses (2020 to November 30, 2020) (BC Coroner stats).
Horgan indicated that he takes pride in BC public health having “asked people to use their common sense” during the pandemic this year.
“We’re not playing around here, this is serious business,” said Horgan about the pandemic in a tone and vernacular that has only very recently emerged in political and public health delivery.
Until very recently the delivery has focused on detailed epidemiology that has required a lot of focused thinking on the part of people who may not normally process scientific concepts in their daily lives. That has no doubt been a necessary level of public education, but in many ways it was delivered with an assumption that people already understood “it’s a virus” (as if to say, don’t you realize how small viruses are, how easily they can spread, that they are not even technically a lifeform and their only purpose is to replicate — in this case using human bodies for that purpose).
To compare the severity of the impact of a widespread relentless virus on the entire population (including social conventions, economy and financial sustainability) to a ‘zombie apocalypse’ would not have been unrealistic, though it would have seemed dramatic, to be sure. Perhaps the near-daily and now continuing pretty-much bi-weekly media announcements about COVID certainly underscored the crisis. But to leave the gut-level communications strategy to nearly a full year into the pandemic could be seen as a point of oversight.
COVID response in frontline acute care:
When the pandemic first wave was upon us, BC public health had looked to what was happening in hard-hit jurisdictions (such as Italy where there was massive COVID spread and a high death toll), and now admittedly over-reacted. Conditions were not the same here in Canada (and particularly in BC) in terms of:
- population density (and systems to support that),
- living conditions (how tightly packed, how many people per household, how well serviced for ventilation and water),
- air quality (longstanding pollution over years that would have pre-reduced people’s health resilience against respiratory infection),
- overall age of population (skewing the numbers as to the severity of impact on frontline health-care), and
- overall level of preparedness on many social and public health levels. BC was in a better position in all instances.
Surgical renewal strategy:
During the surgical shutdown, a lot of people with non-COVID but serious conditions went without scheduled or required surgeries. Though the silver lining was the downtime opportunity for the system to streamline itself and prepare for an even more efficient delivery system after reopening, as implied by the Premier today.

And now (as Health Minister Adrian Dix has frequently pointed out in COVID media updates) more surgeries than ever are being done as part of the BC surgical renewal program that was launched in May, reported on in detail in July, and continues on now through to year-end and beyond.
This concern for the load being put onto the frontline health care system is not new, and not exclusive to Island Social Trends. When the surgical renewal was first launched, and since, there have been the occasional questions from long-time members of the legislative press gallery, including Vaughan Palmer (Vancouver Sun) and Les Leyne (Times Colonist). No one has pushed too hard yet; these are trying times and there is sensibility about not wanting to fuel the fire of burden — but there has always been a sense of knowing that this push cannot be sustained indefinitely.
Island Social Trends has had a media question in the queue for weeks on this, in particular as to the impact on the well-being (resilience of) doctors, nurses and other health care personnel — specifically as to the system’s ability to maintain a full-throttle pace. The system is only as strong as the performance of the personnel. All the equipment, systems and schedules in the world are irrelevant if there are no people and expertise to power them.
Beyond ‘banging pots’:
People have been asked to ‘bang pots’ and show our appreciation for frontline health-care with touching moments of gratitude with hearts and flowers. But are frontline health care workers getting scheduled breaks (additional days off) as a way to pace their resilience on the front lines? Are they getting additional ‘danger pay’? Are they regularly assured of adequate supplies of personal protective equipment (PPE)? Are they getting regularized professional or system support for mental and emotional well-being (as part of their work week)?
It’s about system resilience:

Naturally there is concern for the health-care workers themselves, and indeed the operation of the hospital and acute care system. But why this matters to British Columbians is because if we do need the support of the frontline health care system, how reliable will it be.
There is natural ebb and flow in life. Is there going to be a followup later on for the use of vacation days that have perhaps been missed during this COVID overload period (and how will that impact the delivery of services at some future point — where is the natural pause)?
When do things begin to fray around the edges, if they haven’t already? On Christmas Day there was news of an outbreak at Vancouver General Hospital — the largest acute care facility in the province where multiple patients tested positive for the disease (impacting for now just the respiratory unit T12A which is now closed to new admissions, transfers and visitations).
There was lower than normal pre-Christmas attendance in emergency rooms last week, said Dix in a media session, and he seemed surprised. But if people have postponed ER visits in whatever manner (actually not so urgent, and can wait until after Christmas), that’s not surprising given that few people want to take the risk to end up in hospital over Christmas. Perhaps this was a gift of British Columbians to health-care workers, to lighten their load ahead of the only province-wide break we can all have on this Christmas/Boxing Day weekend.
Getting more answers:
So far, there’s been no luck for Island Social Trends in the bi-weekly live media Q&A on getting some specific answers on this matter. So as of December 23 this question is with BC Health Communications via email, and we look forward to an answer after the holiday break.
In the days ahead of Christmas break (on the day BC’s top doctor and Island Health’s top doctor got their first dose of the mRNA-type COVID vaccine) we did ask this question of Island Health Chief Medical Health Officer Dr Richard Stanwick. Part of his reply was was to say that ‘chocolates are a nice gesture’ but people should just stay home at Christmas as a way to not spread COVID and put further burden on health care. Indeed, this is a provincial-level issue, and the cute gestures of first-wave COVID are really perhaps now a bit stale.

Where Island Social Trends is going with this is that perhaps there should be additional compensation for health care personnel working under duress and essentially non-stop for an extended period. Or perhaps there is, and government is reluctant to float this into the news. This is a high-level budget issue and will no doubt open some issues with unionized personnel. Therefore, no surprise on a lack of specifics from the government on this.
Pause and regroup:
We hear, in the COVID media sessions, Minister Dix’s pride on how hard the hospital frontline workers are doing, and the performance of the system overall. No one is ungrateful about this commitment. British Columbians are fortunate for the level of hospital and acute care services in this province, and most people know that.
But it’s a relatively easy observation that any system operating at full-throttle has to find a pause point, if only to regroup and muster up the resilience for another round. In fact, that pause-point might best have come in the summer in the very realistic expectation of this second wave that even Provincial Health Officer Dr Bonnie Henry said she was surprised had come on so strong (case numbers and spread hit a peak in mid-November).

Overwhelm in every aspect of society and living has been a reality throughout the pandemic in BC this year, indeed everywhere in Canada and beyond. So this is not a criticism but a thoughtful inquiry as to when will the health care system take the time — a moment’s pause — to retool for the first portion of 2021 (and the rest of 2021, in various phases). Panic mode is evidenced by pushing too hard; management is evidenced by deliberate pauses for reassessment toward the best possible effective action going forward.
Preparing for a third wave:
There could even be a third wave in January and February in BC (“in our pandemic” as Dr Henry likes to frame the management of COVID-19 in this province). Globally, a third wave is already said to have begun at mid-November — in BC that’s when we saw a peak in COVID cases, in our second wave.
A third wave will have not only an increase in COVID-19 cases (including the challenge of mutations in the virus and the concomitant challenge of adapting the available vaccines), but will happen under conditions in which frontline workers are truly very worn and the general public is starting to let their guard down due to COVID-fatigue.
It will soon have been a year since the virus reached our shores (originally arriving in BC due to people who had travelled abroad and returned home to BC). Dr Stanwick — even on Vancouver Island where COVID numbers have been comparatively low — is “worried about January”.
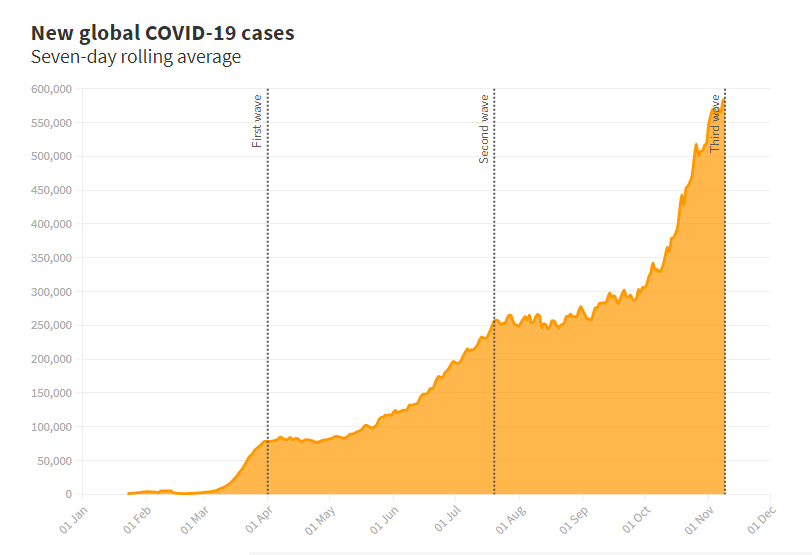
Globally-speaking, the US has by most parameters, entered its third wave while India and Brazil seem to still be on one big wave.
The key parameters for the management of subsequent waves of COVID-19 seem to be the effectiveness and/or intervention of governments and public health in terms of eliciting appropriate (results-oriented) responses from the population in terms of reducing spread and also frontline health-care in terms of resources (including personnel).
Management of personnel and vaccination:

As more frontline health-care personnel become worn out (and also infected by the disease itself), the personnel side of the COVID-response equation becomes increasingly challenged.
No doubt the public health prioritization of COVID vaccines going first to frontline health care workers is the obvious, sensible and urgent thing to do. As per BC CDC stats at December 24, the mRNA COVID vaccine (by Pfizer-BioNTech) had been administered to 8,178 people in BC (almost entire frontline health care workers).
One expects that government leaders, public health and the frontline health-care system knows this tougher, rougher phase of on-the-ground pandemic realities is right around the corner.
But if we could hear more of the nitty-gritty details from our political leaders on this matter of frontline health-care management, it might help the worried, the fatigued, the overworked, and the fearful to rest just a bit easier heading into the 2021 backstretch of this long COVID endurance race.

===== About the writer:

Island Social Trends editor Mary P Brooke, B.Sc. has been covering the political and public health aspects of the COVID-19 pandemic all year as part of the mainstream media coverage of the pandemic.
Island Social Trends is the current flavour of Ms Brooke’s socioeconomic examination of society (through a lens of south Vancouver Island and BC), within a thread of reporting on local and regional news. In 2021, this venture heads into our 13th year of current-issues publishing (during 2008 to earlier in 2020 we previously operated at MapleLine Magazine, Sooke Voice News, and West Shore Voice News).