Monday May 4, 2020 ~ BC
by Mary Brooke, B.Sc. ~ West Shore Voice News
There was much anticipation about today’s COVID-19 data modelling presentation, the third in a series so far. We’re on the crest of learning what ‘the new normal’ is during the continued pandemic.
These data modelling presentations are a more detailed way of informing the public about the data-driven reasons behind the approach to managing the COVID-19 pandemic in BC, or as Provincial Health Officer Dr Bonnie Henry calls it almost affectionately: “our pandemic”.
The first two data-modelling exercises were reviewed in-depth with media ahead of public presentation by the Provincial Health Officer (PHO). Those were on March 27 when the pandemic was newly raw, and on April 17 when British Columbians were immersed in a myriad of lifestyle changes that were evidently colliding with socioeconomic norms.
No pre-event briefing for media today:
So it was both something of a relief while also being something of a surprise that there was no intense technical briefing for media ahead of the 1:30 pm public unveiling of the current modeling by the PHO today May 4.
Does this mean we are tired of hearing the details, or that we are somehow in the calm eye of the storm, of that things might soon get better and we’ve already missed an identified turning point?
In a way it felt like ‘not enough’, but in another way it means we are surfing the COVID-19 wave… media (and hopefully by default the public) are in the groove… hearing and understanding the information in ways we can immediately integrate into our daily lives of self-protection against the virus, and somehow also knowing we are clearly not through this yet (so just a bit more information each day is palatable).
Premier John Horgan is set to join BC Health Minister Adrian Dix and Dr Henry in a joint media conference on Wednesday May 6 (at 3 pm) to reveal more about the ‘new normal’ for the summer of 2020. Dix called it a “going forward strategy”.
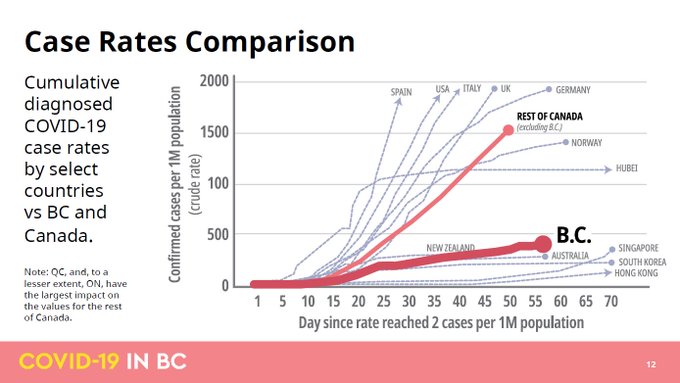
But Dr Henry did say she feels BC is “at the end of our beginning” of the COVID-19 pandemic in BC. We have flattened the curve.
The new normal starts with a ‘unique summer’:
The new-normal preview today was a light touch. Overall concepts were given, with information not entirely big on numbers. The main messages for the overall experience of COVID-19 by British Columbians is that this will be a “unique summer”.

In summary, here are some of the key factors:
- People will be able to get outdoors and gather in small groups but there will still need to be strict adherence to physical distancing as part of “keeping our curve flat”.
- Big sporting events — if any — will probably just be broadcasted, without an audience in the stands. Sports like hockey (which include a face shield) are more likely to relaunch sooner than, say, soccer which is generally unprotected.
- The virus is still with us. We are learning to live with it, until such time as there are effective treatments or possibly eventually a vaccine that is effective and widely available.
- Outbreaks are still ongoing in long-term care, assisted living and acute care facilities, as well as in other communal settings where the virus has spread (such as poultry processing plants and also the prison near Mission). There is always the possibility of spread from those scenarios into associated worker and family populations.
- The outbreak and exposure at the Kearl Lake oil sands production plant in Alberta (with workers from BC returning with infection or possible infection) is of continued concern. One BC health care worker has become infected as a result. Anyone who has had contact or possible contact with someone who has worked there and has returned to BC should be attentive.
A few key epidemiological trends (to April 30):

On the more epidemiological side of things — i.e. who gets sick and maybe why, by the numbers — here are some key points from today’s presentation:
- Most of the 117 deaths in BC to date have happened in people over age 70, right up to age 90. This reflects where most of the infections have occurred (i.e. in long-term care, assisted living and acute care facilities).
- Older men (over age 50) seem to be more susceptible to intense experience with the disease (including more hospitalization and deaths). This may have to do with how the male body’s immune system responds to invasive infection as well as the influence of the COVID-19 virus on clotting receptors on arteries and the heart, says Dr Henry, but that worldwide observation of this phenomenon has not yet found a conclusive reason. It could be that men have more possibly-undetected medical conditions related to work/life stress or use of alcohol as part of certain lifestyles, which could impact the body’s overall ability to combat a sudden infection.
- Severe illness is also prevalent among people with chronic underlying health conditions such as diabetes and underlying heart or lung disease. Having one chronic condition comprised 37% (over one-third) of all cases, and two-thirds of those who were admitted to hospital for COVID-19, where three-quarters of those required ICU. Of those with underlying illnesses in chronic care, 83% died.
- In BC, the overall profile of men’s illness with COVID-19: 44% of all cases are male (so more women than men are catching COVID-19, which has a lot to do with the gender profile among long-term care homes and workers in long-term and assisted living care). Two-thirds of cases that end up in hospital or intensive care are men, and three-quarters of deaths are of men.
- Of the 199 people who have required critical care (ICU) in hospital, 28 (or 14%) died. “That’s a very high number,” said Dr Henry. “It was mainly men over age 50 who’ve had underlying conditions.
- How many have recovered. Of the 199 people in hospital, now 110 of those have been released and have recovered. “A number in between are still in recovery,” said Dr Henry.
- Dr Henry reported today first time about something called ‘excess deaths’. This is a measure of the number of deaths beyond the average. The average number of days per day in BC is 115 deaths (from old age, motor vehicle crashes, and drug overdose). An example of ‘excess deaths’ from 2017 and 2018 was after the very poor air quality in BC due to the intense forest fire season in summer in both of those years due to additional lung and breathing issues. Dr Henry says there have been 170 excess deaths since March, of which 111 so far have been attributed to COVID-19. “This gives us a measure that this outbreak has had a population effect. We don’t know what else is causing these excess deaths during that period of time,” she said, though details from Vital Statistics will shed more light on the tale, in time, based on death certificates. However, Dr Henry says it is possible that (as seen in reduced numbers of people coming into hospital emergency departments) that people with other serious health issues are avoiding hospitals during COVID-19, in some cases leading to death.
Health care workers have become infected:
And we should of course take note about the impact of COVID-19 on health care workers in BC. “Health care workers have been affected — all health care workers,” said Dr Henry today.

She listed off dentists and dental assistants, nurses, psychiatric workers, physiotherapists and care workers.
“Many have been affected at work – either from colleagues or from caring for patients,” she said. “That includes people whose exposures may have been through travel (e.g. the international dental conference that was held in Vancouver), or exposure to family members,” she said.
As of April 28, the total number of cases of COVID-19 among health care workers in BC has been 21% of test positive cases. “Thankfully a very small proportion of those have been hospitalized (8%),” said Dr Henry, but adding that three percent did require care in ICU, and that one health care worker in BC has died due to COVID-19.
Otherwise, most of the health care workers are “younger in age, and female, and did very well — they had milder illness,.” said Dr Henry today.
COVID-19 statistics at May 4:
In BC as of noon today, two 24-hour reporting periods were covered: May 2 to May 3, and May 3 through to midday May 4.
There were 53 new cases confirmed in the last 48 hours: 34 new cases May 2 to 3, for a total of 2,205 cases in British Columbia, and 19 new cases May 3 to 4, bringing the provincial total to 2,224.
COVID-19 is seen in each of the five health regions in BC. Presently the tally shows 845 in Vancouver Coastal Health, 1,027 in Fraser Health, 124 in Island Health, 177 in Interior Health, and 51 in Northern Health.
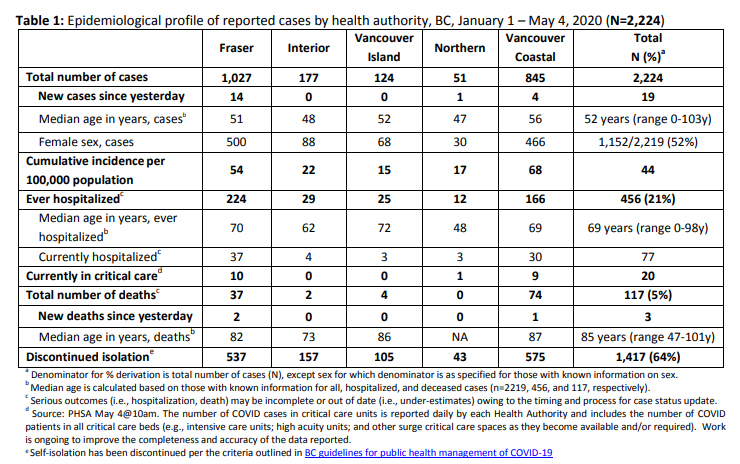
Three more deaths were reported today: two in Fraser Health and one in Vancouver Coastal Health. Both among people infected while in long-term care.
The total number of deaths in BC due to COVID-19 now at May 4 is 117. BC CDC stats (see table above) show that as five percent of people who have tested positive for COVID-19. But to put that in context, there are likely as many as 20 times the actual number of infections of COVID-19 out in the community that have not become part of the tally of ‘test-positive cases’. That would include people who have very mild symptoms who do not seek medical care, and people who are infected but have no symptoms (i.e. asymptomatic).
No new long-term care or assisted-living facility outbreaks in the last day. In total, 19 facilities and three acute-care units have active outbreaks, with outbreaks now declared over at 14 care facilities (total of 33 facilities affected during the pandemic in BC so far).
“Public health teams are also providing support to a number of community outbreaks, actively contact tracing those who may be directly affected and their close contacts.
There are seven confirmed positive cases at Fraser Valley Specialty Poultry, 54 at Superior Poultry in Coquitlam and 35 employees confirmed positive at United Poultry in Vancouver.
“There are also 134 inmates and staff confirmed positive at the Mission Institution federal correctional centre, as well as 15 positive cases of COVID-19 connected to the Kearl Lake plant in Alberta.
To date, 1,417 people who had tested positive for COVID-19 have recovered. Of those, 77 individuals are hospitalized (20 of which are in intensive care). The remaining people with COVID-19 are recovering at home in self-isolation.
Hospital capacity and ventilator equipment:

Today Health Minister Adrian Dix talked about hospital capacity to handle cases of COVID-19, and the number of ventilators on hand in hospitals including portable units that can be relocated to where they are needed.
Dix said that in BC there is now “reduced surge capacity from 951 to 704 critical care bed”s. Currently critical care beds for COVID-19 occupy 43% of the 390 total vacant critical care beds in BC, he said; there are 284 in critical care for non COVID-19 reasons.